
- Oliver Parini
- Dr. Tessa Cattermole
Sitting in an unfurnished Burlington studio apartment, 1,500 miles from home, Tessa Cattermole burst into tears.
The Kansas native had arrived a few weeks earlier for a $55,700 job as a first-year resident physician at the University of Vermont Medical Center. She had emptied her bank account, sold blood plasma and even pawned a flute her mother gave her in the fifth grade to pay for the nearly $10,000 move.
Now, she was late on rent. Her first paycheck was still a few days away. It would barely cover the $1,248 bill. She was broke.
"I remember just crying and thinking long and hard about quitting," she said last week.
She didn't. Yet Cattermole said she barely scraped by that first year as rent and $400 student loan payments sapped much of her take-home pay each month. She subsisted on peanut butter and crackers, printed textbooks from the hospital computers instead of buying them, and biked to work at 4 a.m. because she couldn't afford to get her car repaired. All the while, she kept up with her grueling hospital schedule, regularly logging 24-hour shifts.
Resident physicians hold a unique place in medicine, serving as medical trainees and a source of cheap labor for the hospitals that teach them. But as the cost of living in Vermont has skyrocketed, residents at the UVM Medical Center say the arrangement no longer feels mutually beneficial.
Seeking the power to advocate for better pay, they want to form a union. About 240 of the hospital's 352 residents, including Cattermole, signed cards last month in support of organizing. The first-generation college graduate, now a third-year surgical resident, said her experience shows that the hospital's low pay undermines its goal of attracting residents from a greater variety of backgrounds.
"Historically, medicine has been a profession for people who are already privileged," she said. "Now, hospitals, including UVM, are trying to recruit a more diverse workforce. But there aren't support systems in place for those people."
UVM officials claim to have no position on the organizing effort, but their actions suggest otherwise. They declined to recognize the union voluntarily last month, saying they wanted to ensure that all residents had a chance to weigh in. Their decision came even though more than two-thirds of UVM's residents had expressed support for the move. The hospital is now paying a pair of out-of-state "labor consultants" ahead of an election on April 14 that will decide the union's fate. A simple majority is all that's needed to organize.
Dr. Jason Sanders holds leadership roles at the UVM Health Network, including president and CEO of its Medical Group, which oversees doctors across the system's six hospitals. He said the medical center was not trying to dissuade residents from unionizing. "Our focus is on as many residents participating as possible in the election and them having as much information as possible," he said.
Residency, a term that stems from the days when medical trainees lived at hospitals, is usually their last step before becoming fully licensed doctors. The gigs last three to seven years, depending on the specialty.
Medical school graduates have very little control over where they serve their residencies. They submit a list of preferred hospitals to a private nonprofit that then assigns them to one of the nation's 1,000-plus teaching hospitals. At an annual event known as Match Day, every graduating doctor in the country opens an envelope to learn their fate.
It is difficult for residents to transfer once they have been matched, so hospitals have less incentive to compete on pay or working conditions. And residents are reluctant to complain once they arrive at their assigned hospitals, aware of their status in the hierarchical world of medicine.
They work long shifts with little sleep. While the federal government has capped weekly hours at 80, that's just a monthly average — many residents say they regularly exceed that total. The UVM Medical Center even has a policy titled "Fatigue Management" that offers practical tips about naps and "strategic" caffeine use. Studies estimate that nearly 30 percent of residents in the U.S. go on to experience symptoms of depression during their training.
As they learn more, they become part of a "critical" workforce at teaching hospitals, said Dr. Candice Chen, a professor at Georgetown University's Fitzhugh Mullan Institute for Health Workforce Equity. They ensure that patients get the care they need, she said.
Despite the job challenges, only about one-seventh of the 145,000 resident physicians in the U.S. are unionized. Many are represented by the Committee of Interns and Residents, a New York-based union working with the UVM residents.
Organizing efforts ramped up during the pandemic as doctors-in-training found themselves on the front line of the life-altering public health crisis. Several residency programs unionized last year, while another drive is under way at Stanford Medical Center in Palo Alto, Calif.
UVM residents began drumming up support last fall. Dr. Hannah Porter, a second-year dermatology resident who is one of the union drive's leading voices, said many of her colleagues were initially wary, fearful that union involvement might jeopardize their future job prospects.
But they came around after seeing how resident unions have succeeded elsewhere, she said. Those victories include double-digit salary bumps, housing and meal stipends, and guaranteed slots at hospital-run childcare centers. One residents' union, at the Institute for Family Health in New York City, even negotiated the nation's first-ever 70-hour maximum workweek. "It was really about showing the evidence that this actually can be great for us," Porter said.
Organizers say their union would initially target UVM's compensation package, noting that they are among the lowest-paid doctors in the region: A first-year at UVM earns $60,000, trailing their counterparts at the Maine Medical Center ($63,000), Dartmouth-Hitchcock ($63,600) and the Albany Medical Center ($68,000).
Sixty thousand dollars would be considered a decent living in many professions. But the typical doctor leaves medical school with about $200,000 of debt, and a pandemic-era pause on student loan payments could lapse later this year.
That means many residents will suddenly have to pay $300 to $500 a month, Cattermole said. "That's a huge chunk of our income," she said.
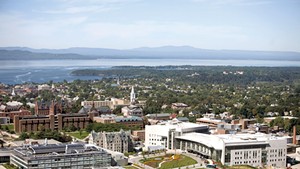
UVM residents also usually try to live near the hospital, which is located in Vermont's most expensive county. That's if they can find a place: The county's rental vacancy rate dipped below 1 percent last fall. Some first-year residents ended up living in hotels because they were unable to find an apartment, according to Dr. Taylor Haring, a second-year anesthesiology resident.
"You're working 80 hours a week at a hospital, then coming home to a hotel room and have to look for an apartment or house?" Haring said. "We want to be focusing on patient care, not worrying about paying rent or buying groceries."
Residents say they also want housing stipends, raises tied to inflation and a better parental leave policy. Currently, only new mothers can take paid time off — six weeks for a vaginal birth and eight if they have a cesarean section.
Medicare reimburses teaching hospitals some of the cost of training residents. At the UVM Medical Center, almost three-fourths of the hospital's residents are federally funded. The hospital is receiving about $34 million this year, or 70 percent of what it costs to run the entire residency program.
Hospital leaders say they evaluate resident pay and benefits when drafting the budget each year and note that resident pay has increased 10 percent over the last five years.
Sanders, the health network executive, said officials review feedback from an annual survey that includes questions about compensation. A resident-led committee also regularly interacts with the hospital, he said.
But residents on that committee say almost all their requests have been shot down with little or no explanation. Cattermole, the chair, said she asked for a meeting with hospital leadership about compensation months ago and never heard back. "It just feels like there's no way to advocate for ourselves," she said.
The unionization push comes at a time of uncertainty for Vermont's only teaching hospital, which is currently staring down a nearly $40 million budget gap. Officials say the losses are driven largely by labor expenses associated with temporary traveling workers. They've asked state regulators for permission to reopen this year's commercial insurance fee structure to hike it by an additional 10 percent and say they will likely seek another major increase next year.
"We're in dangerous water," Al Gobeille, the health network's executive vice president for operations, said at a hearing last week.
UVM's leaders have resisted weighing in publicly on the effort. That doesn't mean they're taking a hands-off approach, though.
Two Massachusetts-based labor consultants have been working with the hospital for the last few weeks: Carol Holland, a former executive at a major health system who is now president of Compass Healthcare Advisors; and Katie Lev, the former director of labor relations at CVS who now runs her own consulting firm, Lev Labor.
Holland has a limited track record; she's only three years into her consulting life, according to her LinkedIn bio. Lev, meanwhile, has worked for employers in several high-profile unionization efforts, including online legal news outlet Law360, which tried to defeat a union drive six years ago. In a talk with the outlet's staff that was recorded and shared with HuffPost, Lev repeatedly questioned the benefits of a union and encouraged the journalists to give management a chance to remedy their problems.
The hospital has instructed the consultants not to interact directly with residents, according to Sanders. He said they are on hand simply to help attending doctors — who supervise residents — navigate the campaign, since most have no practical experience with the process and aren't sure what they can and cannot say.
Residents, however, said they have noticed a difference since the consultants came aboard. Several said that attending physicians who previously expressed support for their union now seem to be sticking to a script.
The hospital has also disseminated information about unions directly to residents, including material that organizers say is misleading. A six-page FAQ, for example, warns residents that they would no longer be able to individually negotiate terms of employment with the hospital if they unionized. But in fact, that is something they already cannot do, organizers say.
Cattermole, the surgical resident, said she is in a much more stable position today. She now lives with her partner, with whom she shares the rent, and the two have managed to save enough money to buy a house. She expects to join the 40 percent of residents who go on to work for the hospital after their training.
"I'm one of those people who fell in love with Vermont," she said.
Still, she worries about the next crop of UVM residents, particularly those who, like her, come from less advantaged backgrounds.
"If you truly value a diverse workforce with people from different backgrounds," she said, "you can't stick with the same system that you always have. It's obviously not working for us."
Correction: A previous version of this story misstated Dr. Hannah Porter's post-graduate year.













Comments
Comments are closed.
From 2014-2020, Seven Days allowed readers to comment on all stories posted on our website. While we've appreciated the suggestions and insights, right now Seven Days is prioritizing our core mission — producing high-quality, responsible local journalism — over moderating online debates between readers.
To criticize, correct or praise our reporting, please send us a letter to the editor or send us a tip. We’ll check it out and report the results.
Online comments may return when we have better tech tools for managing them. Thanks for reading.